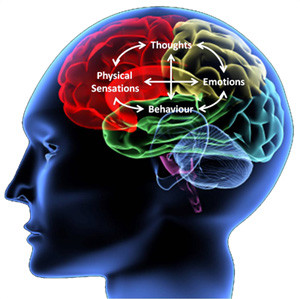
What is Cognitive Behavioral Therapy?
by Counseling and Wellness Center of PittsburghMarch 4, 2019 Behavior Therapy, CBT, cognitive behavior therapy, Cognitive behavior therapy near me, cognitive distortions, Cognitive therapy, maladaptive assumptions0 comments
Cognitive Behavioral Therapy, or CBT, is a common buzz word and psychological term, but what is Cognitive Behavioral Therapy? According to the Beck Institute, In clinical terms, it is a specific theoretical therapy that is used as a psychological treatment. Since its creation in the 1960’s by Dr. Aaron Beck, CBT has been proven to help reduce the symptoms associated with a range of...Learn MoreMeditation, The Number One Mistake Beginners Make
by Counseling and Wellness Center of PittsburghApril 19, 2018 counseling, meditation, mindfulness, therapy, wellness0 comments
Meditation and Mindfulness
Want to Become a Meditation Master? This is the Most Common Mistake that New Meditators Make and How to Fix It!
So maybe you have read the abundant data that meditation is one of the most fantastic tools that there is to enhancing mental clarity, reducing individual response to stress, and enjoyment of the great benefit of greater calm. According to the National...Learn MoreAgoraphobia
by Counseling and Wellness Center of PittsburghApril 3, 2018 agoraphobia, anxiety, anxiety therapy pittsburgh, counseling for anxiety, counseling pittsburgh, help for anxiety, panic attack, therapist, therapists, therapy, Therapy and Counseling For Anxiety0 comments
Agoraphobia
Agoraphobia is a type of anxiety disorder that can sometimes co-occur with panic disorder. Its prevalence rate in the population is low, occurring in only about 1.1% of the population. Agoraphobia is hallmarked by a fear of leaving the house or other safe place. This often cooccurs with panic attack or panic disorder because a person has experienced a panic attack and then fears...Learn MorePost Traumatic Stress Disorder Therapy and Counseling
by Counseling and Wellness Center of PittsburghApril 1, 2018 anxiety, anxiety therapy pittsburgh, cognitive behavioral therapy, counseling, counseling for anxiety, counseling pittsburgh, help for anxiety, licensed therapist monroeville, licensed therapist pittsburgh, post traumatic stress disorder, ptsd, searching for a therapist in monroeville, searching for a therapist pittsburgh, therapy, Therapy and Counseling For Anxiety0 comments
Post-Traumatic Stress Disorder
Post-Traumatic Stress Disorder is a form of anxiety disorder which stems from exposure to a traumatic event or situation which caused real or threatened injury to and this can also be caused by the witnessing of an event or situation which injured or threatened injury to another person. According to the DSM IV, there is a lifetime prevalence rate of about 8% for...Learn MoreObsessive Compulsive Disorder OCD, Therapy and Counseling
by Counseling and Wellness Center of PittsburghMarch 16, 2018 anxiety, anxiety therapy pittsburgh, cognitive behavioral therapy, counseling, counseling for anxiety, counseling pittsburgh, generalized anxiety disorder therapy pittsburgh, Help for obsessive compulsive disorder, licensed therapist monroeville, licensed therapist pittsburgh, obsessive compulsive disorder, OCD, searching for a therapist in monroeville, searching for a therapist pittsburgh, therapist in murrysville, therapists, therapy, Therapy and Counseling For Anxiety, therapy for anxiety, therapy pittsburgh0 comments
Obsessive Compulsive Disorder
Obsessive compulsive disorder is a type of anxiety disorder which afflicts .5-2.5% of the population. The disorder greatly effects the quality of life for the sufferer and becomes a consuming pattern of anxieties and rituals which are centered around both obsessional worries and compulsive behaviors. Most of the individuals who have this disorder at one time or...Learn MorePanic Attacks and Panic Disorder
by Counseling and Wellness Center of PittsburghMarch 16, 2018 anxiety, anxiety therapy pittsburgh, cognitive behavioral therapy, counseling, counseling for anxiety, counseling pittsburgh, generalized anxiety disorder therapy pittsburgh, licensed therapist monroeville, licensed therapist pittsburgh, searching for a therapist in monroeville, searching for a therapist pittsburgh, therapist, therapy, therapy for anxiety, therapy pittsburgh, wellness, wellness center monroeville, wellness pittsburgh0 comments
Panic Attacks and Panic Disorder
As many as 4.7% of people will experience a panic attack at some point in their lives, panic disorder is a form of anxiety disorder which can be extremely intense, many times individuals who have a panic attack end up going to the emergency room imagining that the rapid heart beat and dizziness are a heart attack. Symptoms and features of anxiety disorder...Learn More